Clostridioides difficile infection – an experience report
Why does this page exist?
This page was created because I had to fight a Clostridioides infection myself. During this time I have gone through death fears and went through hell. The reason for this was on the one hand that with each therapy the probability is quite high that one suffers a relapse – also with me. For months I trembled whether I would ever be able to get rid of these bacteria and lead a normal life again. On the other hand I had to experience that an infection with Clostridioides Difficile brings most doctors to the limits of their knowledge. The disease is usually so rare that neither my family doctors nor internists knew what to do with me.
This is because it is a disease that usually occurs in older people in clinics. They are usually the result of antibiotic therapy, or because some patients only have a very weak immune system. I have to add at this point that an employee in our regular pharmacy said that she has been experiencing an increasing number of cases recently. She assumes that this is because doctors prescribe antibiotics far too often, although they are not always necessary.
In any case, I would like to make it clear that this is not a reproach to school doctors. In the end, I managed to get the disease under control again with the help of the findings of orthodox medicine. Unfortunately, however, many people affected by the disease encounter doctors who simply lack the necessary experience in this field when they are confronted with this infection. I had to research and read a lot until I had an idea of what was actually happening in the intestines. So I put the puzzle together myself as a patient.
On this page I would therefore like to describe to you how the successful therapy came about with me. Of course this is no guarantee that it will be the same for everyone else. But nevertheless I have used some aids which probably supported the healing and which are not part of the usual treatment plan. I would like to emphasize that NO HOMEOOPATHY has been used during my cure.
With this site I hope I can help you to recover faster and avoid relapses with Clostridioides.
For reasons of data protection I don’t want to mention my name. By the way, it is not the one you can find in the imprint. Peter only made it possible for me to put my story on paper.
Another point: you should know that I´m German. So please don´t be irritated if I sometimes use the wrong terms and expressions. Try to see the ide behind it.
Clostridioides Difficile – the disease begins
You should know, I’m not a doctor. Therefore, I cannot speak too expertly about some medical details related to the disease. However, it is very important to understand some basic things about the intestinal flora and the properties of bacteria so that you can understand why the therapy worked for me in the end.
Here is the most important info first:
A dieseas due to Clostridioides Difficile is usually caused by antibiotics
My infection was like this: it was winter. In the period between January and March everything gasps and flies as usual. I had a bad bacterial tonsillitis. In March 2018 I was prescribed the antibiotic CEFUROXIM. Later, after I still had problems, I was misdiagnosed by a clinic doctor. She diagnosed lymph node inflammation even though there was no indication of it in the blood count. She prescribed the antibiotic CLINDASOL. Two other doctors, the house etcher and an ENT doctor, questioned this verdict and advised me to stop the CLINDASOL immediately. But it was already too late.
Because of the 2 different antibiotics within a relatively short time, it is not 100% clear which of them caused the damage. My general practitioner and I, we are betting on the CLINDASOL.
Important for you: My doctors told me afterwards that it is often the antibiotics that begin with “C” that trigger the disease. Also some broad-spectrum antibiotics and penicillins. For this there is a list of risk assessments – with which certain antibiotics trigger the disease. To see in the picture: CIPROFLOXACIN
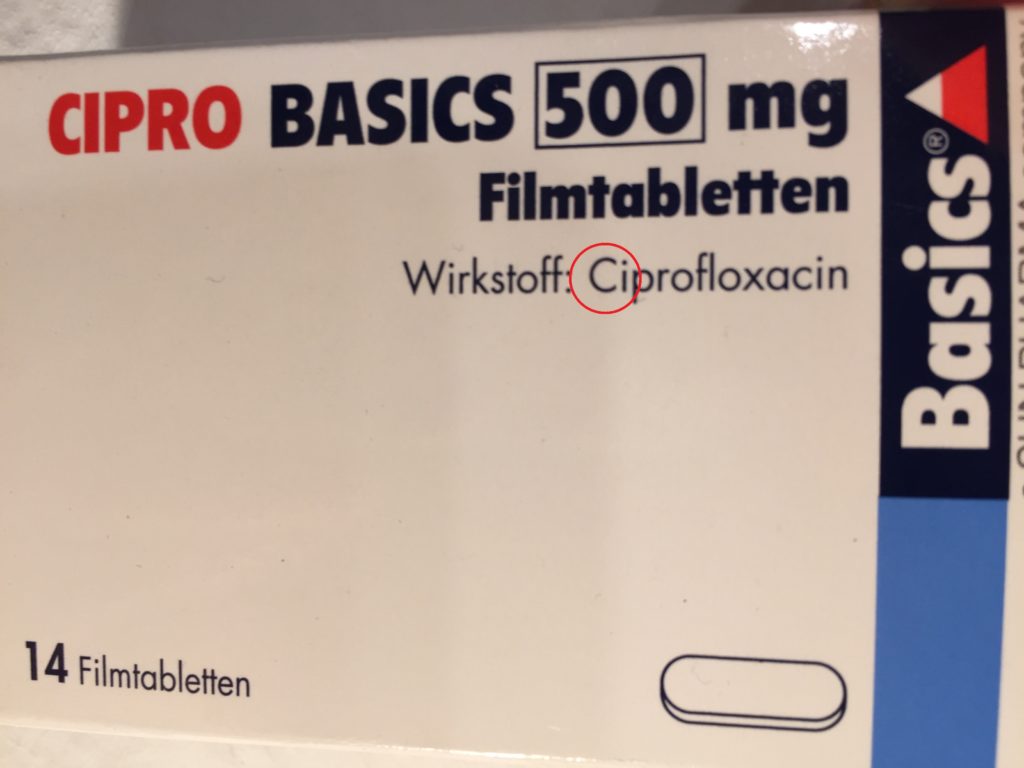
Here is an overview for the antibiotics, that can cause a Clostridioides diesease:
High risk: clindamycin (contains the mentioned CLINDASOL), second and third generation cephalosporins (contains CEFUROXIM), fluoroquinolones (CIPROFLOXACIN, moxifloxacin, levofloxacin), ampicillin, amoxicillin
Medium risk: trimethoprim, tetracyclines, imipenem, meropenem
Low risk: aminoglycosides, macrolides (especially: clarithromycin, azithromycin), broad spectrum penicillins, ticarcillin, mezlocillin and piperacillin, VANCOMYCIN.
The reason for this process is that Clostridioides is not an “infection”, but has usually always been present in the body. Antibiotics only bring them to “power” in the intestine. How that works, more about that later…
The first signs that something was wrong were the penetrating pain on my left side of my stomach. They just didn’t go away and I was very worried. No family doctor at that time had the idea that there might be something serious behind it. I shouldn’t worry, it could be flatulence or maybe a small intestinal infection.
When things got worse and worse over time, the doctor of the emergency medical service was in our apartment once at night. He had been the first to clearly warn that there could be a serious danger in the intestinal tract after antibiotic therapy. He asked whether nobody had taken a stool sample from me before. That would actually be standard if someone had intestinal pain? Well, unfortunately no. Because it is probably the case that in 80% of the cases the pain actually disappears on its own. That’s why many doctors ignore the problem at first and let things run their course. So I gave a stool sample, but almost at the same time I had slimy and bloody diarrhoea. So my condition worsened.
Why do these characteristic symptoms occur?
Clostridioides Difficile Disease – Cause
Clostridioides Difficile are anaerobic bacteria, which are mostly part of the natural intestinal flora. Anaerobic means that they do not process oxygen for the metabolism.
A special feature is that they have the ability to encapsulate themselves and form spores. In this phase, they are virtually invulnerable to drugs. This circumstance will be very important later when I describe the course of the long-term therapy.
Clostridioides are typical hospital germs. They often infect elderly patients in medical facilities whose immune system is weakened. Therefore the lethality rate reaches 1-2%, whereby it is many times higher with older patients.

It is important to know that Clostridioides are completely harmless in healthy people as long as their population remains in normal proportion to the number of other intestinal bacteria. But, some strains of Clostridioides produce toxins. Their amount is actually too small to cause harm to humans.
However, the problem begins as soon as certain antibiotics enter the body. Antibiotics are known to kill harmful bacteria. In this way they free us from dangerous pathogens. Unfortunately, they also often work against many of the good bacteria that are present in our intestines and which we actually urgently need to be able to digest food. This complex eco-system is completely turned upside down by the intake of antibiotics…
The destruction of the intestinal flora by antibiotics
Imagine that: There is a colorful, varied cocktail in our intestines, which is composed of a large number of bacterial species and also some fungi. They all form the so-called intestinal flora. Whereby there is a difference between large intestine and small intestine. Here are some important bacterial strains:
Proteolytic bacteria – digest protein: Bacteroides, Proteus, E. coli, Clostridioides
Sacchacholytic bacteria – cleave carbohydrates: Bifidobacterium, Lactobacillus, Streptococcus faecalis
Gram-negative bacteria: E. coli, Proteus, Enterobacter, Serratia, Yersinia, Salmonella.
As long as the composition of the flora is well balanced and no species has the upper hand, everything is fine in the intestinal area.
By the supply of antibiotics many of these intestinal bacteria are decimated in their number. However, not some of the strains of Clostridioides Difficile are resistant to certain antibiotics.
This means that suddenly there is plenty of room for them to spread undisturbed in the intestinal tract. Thus, the Clostridioides start to multiply rapidly. Bacteria grow by cell division. One bacterium becomes two new ones, two become four… etc. It is therefore an exponential growth and not a linear one. The curve at the bottom of the picture shows what happens when the population starts with only one bacterium. You can see that it starts slowly. But after 10 or 11 cell divisions at the latest, the population grows incredibly rapidly. Only when the existing habitat reaches its capacity limit does the curve level off again.
This process is typical for the spread of pathogens in the exponential phase. Therefore, it sometimes takes a few days or even weeks after ingestion until the problems appear.
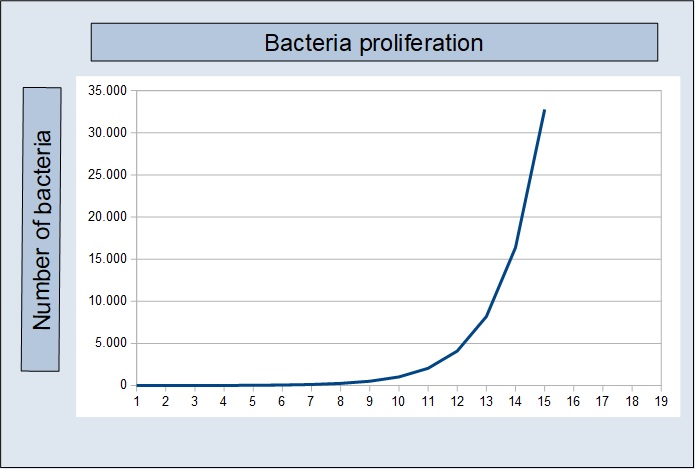
This means: Clostridioides are suddenly in excess in the intestine. Due to their exponential growth, they take away the habitat of other bacterial species and thus prevent their proliferation. The flora can no longer settle into the balanced state.
The fact that some strains of the Clostridioides Difficile bacteria produce toxins makes it dangerous for humans:
- Toxin A (enterotoxin) – causes loss of fluid in the intestine
- Toxin B (cytotoxin) – attacks the cells of the large intestine
If one of the toxins occurs in larger quantities, or both in combination, they cannot be broken down by the body without further ado. Either they cause diarrhoea or they start to “eat away” at the intestinal wall. In the worst case both.
The toxins cause the so-called “pseudomembranous colitis”. This causes the bacteria to decompose the intestine, which can lead to an intestinal rupture. A clear sign of such an attack is a bloody and / or slimy bowel movement. In addition there is a really terrible smell, which you will probably never forget again once you have experienced it.
A hint to these problems can usually be found briefly torn in the package insert of the medication:
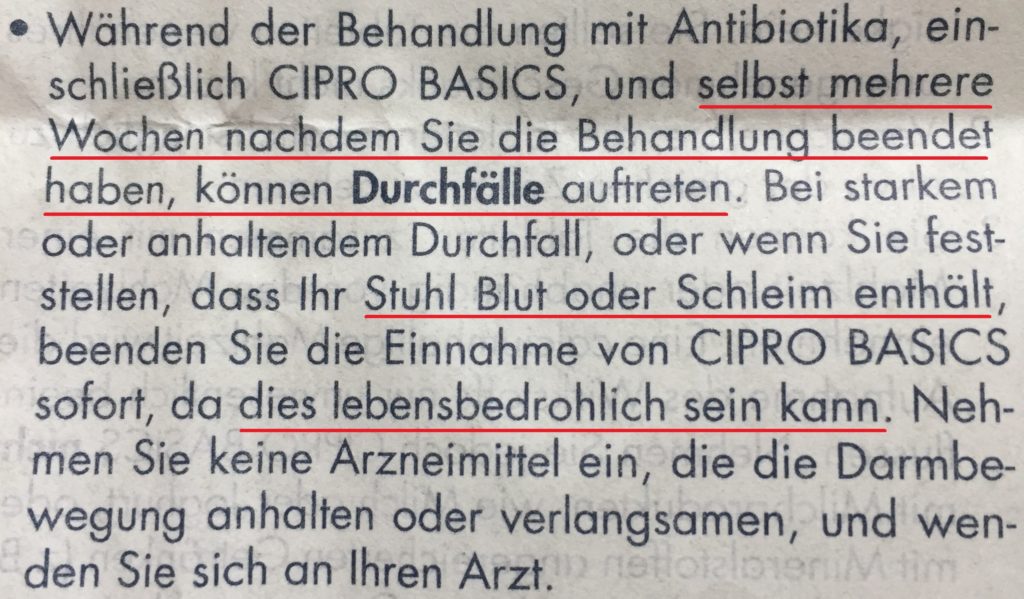
TRANSLATION: It is possible, that even several weeks after the usage of CIPROFLOXACINE, diarrhoea may occur. If your defecation stool should contain blood or slime, please stop using CIPRO immediately.
If the Clostridioides are in such an increased number in the intestinal area, then there is normally almost no chance that a healthy intestinal flora will establish itself on its own. Even with a healthy diet or an artificial supply of bacterial cultures, the probability is virtually non-existent. The amount of Clostridioides is already much too large for this. They would leave the good bacteria no place to establish themselves. Without taking special antibiotics, Clostridioides Difficile would destroy the intestines and cause death over time.
Clostridioides Difficile – Diagnosis
Of course, before doctors start to treat a patient, proof must first be furnished that it is indeed Clostridioides that causes the problems. There are two ways to do this:
- Stool sample with toxin detection
- Colonoscopy – not a standard procedure
Stool sample with toxin detection
The detection of a dangerous Clostridioides infection is usually done with a stool sample. I had to fill a few spoons from my chair into a plastic tube. This was then sent to the laboratory. After about 3-5 working days the result comes. That doesn’t sound like too much time, but if you have slimy diarrhoea and pain while waiting, it feels like eternity. Here is my result from the laboratory:
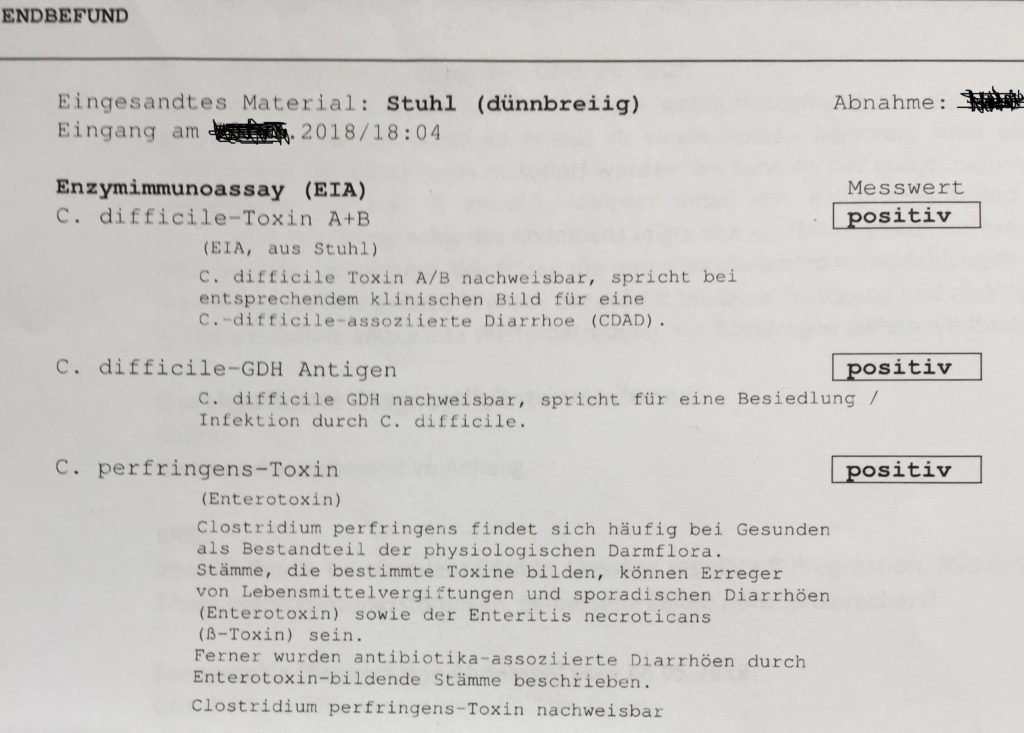
If the sample contains evidence of toxin A and toxin B, then action must be taken. From this point on it was clear that this was a colonization by the dangerous tribes of C. Difficiel. There were even toxins of the variety Clostridioides Perfringens present.
Colonoscopy
A colonoscopy is used to check for the presence of pseudomembranous colitis. The internist can see excessive colonization with Clostridioides in the intestine from a very typical looking white coating.
This means that Clostridioides disease can be detected optically from a certain point in time using this method. However, it is not used to detect the pathogens themselves, but only when the presence of colitis is checked. The stool sample and its evaluation therefore remains the most common method.
Clostridioides – the first therapy
The primary standard therapy against Clostridioides is the antibiotic METRONIDAZOL. This drug is especially effective against anaerobic bacteria. Clostridioides Difficile also belongs to this group. On the other hand also other inhabitants of the intestine. These are also attacked by the remedy.
I don’t know exactly what the legal background is, but it seems that the health insurance companies insist on using this drug for the first infection. The reason: The drug METRONIDAZOL is relatively widespread and costs considerably less than other antibiotics. A pack of 30 tablets is usually available for around 30 euros.
I have to say that METRONIDAZOL had done its job. I had taken it for 10 days and the complaints were gone – for the time being. With many concerning this means seems to be sufficient actually for an ebbing of the problem. Unfortunately, however, relapses occur quite frequently.
With me it was unfortunately in such a way and already after 5 days the symptoms came again. The agonies started all over again. The pain was so severe that I was taken to the hospital by ambulance. I was also very dehydrated because I had lost a lot of fluid due to diarrhoea.
In retrospect, I wonder whether the therapy would not have been permanently effective if I had given my intestines the support I needed to become healthy. In the end, METROMIDAZOL killed the dangerous Clostridioides. Unfortunately, however, these have the property that they can encapsulate themselves when threatened. This protects them from antibiotics. A fading interval therapy might have been more successful from the beginning. In this way, the germs would gradually be caught, and after some time they would free themselves again from their encapsulation.
Clostridioides – 1st relapse
Another stool sample was taken at the clinic. The result was soon clear: Clostridioides toxins – tested positive. This time the diarrhea was slimy and spread this typical, terrible smell, which is hardly bearable. A laboratory assistant later told my general practitioner that you didn’t even need a microscope for some samples because you can sniff out the disgusting stench of Clostrieden quais.
This time, however, the doctors from the clinic approached the matter with a drug that does better in tests for efficacy against Clostridioides. The antibiotic VANCOMYCIN.
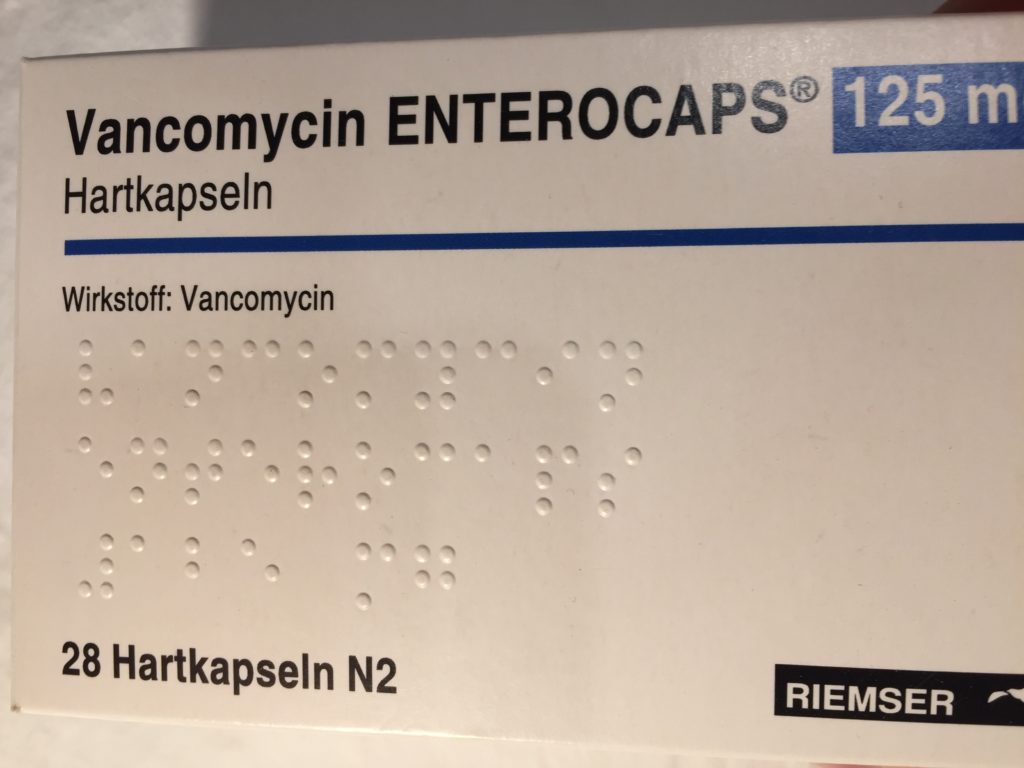
VANCOMYCIN is a quiet modern antibiotic that is significantly more expensive than METRONIDAZOL. In comparison:
- Vancomycin 250 g – 30 pieces: between 400 – 500 EUR
- Metronidazole 400 g – 30 pieces: approx. 30 EUR
Therefore, it would also be clear why the health insurance companies would certainly prefer metronidazole in the first step. But I cannot say whether there are really any regulations on the part of the health insurance funds. Who knows, maybe as a patient you can push for VANCOMYCIN right from the start. You can try it.
The modernized version of VANCOMYCIN is so effective because it is not absorbed by oral administration, but only works in the intestine. In addition, it fights the bacteria simultaneously via three different points of attack. This makes it difficult for germs to build up a resistance against the drug.
On the internet I searched for information on different pages. There was to be read frequently that the relapse ratio is lower than with the METRONIDAZOL. However, these were not sources which I would trust completely. Therefore I stick to what I experienced: VANCOMYCIN was effective and the disease regressed.
Again, I regret that I did not insist on a decaying interval therapy. The people in the hospital didn’t seem to have too much experience with the disease themselves. They just said that it was not necessary, I should think positively … it will be again …
I asked if I could do anything more than just take the antibiotic. If I can do something to promote the intestinal flora. For example, I had heard of Mutaflor. These are capsules containing cultures of certain E. coli bacteria whose presence is important for intestinal health. Or whether I should eat yoghurt? The answer was always something like this: “Yes, why not… can’t hurt…”. But there were no more tips. So at least in this phase I started to take MUTAFLOR. It contains cultures of the E.Coli bacteria stem 1917l in high numbers.

I don´t know if there are equivalent capsules in your country, but MUTAFLOR can be bought on the German AMAZON website and be sent to you.
It was only afterwards that I learned from a friend from my school days (now doctor of chemistry in the pharmaceutical industry) that lactic acid bacteria are very effective in inhibiting the spread of C.Difficile. I should have taken more lactic acid products like buttermilk and kefir. But as I said, some doctors lack experience. As in any other profession, you can’t know everything.
Unfortunately, this therapy did not work either. I took VANCOMYCIN for 10 days. Every day 4 tablets of 125 mg each.
5 days after weaning I got slimy diarrhoea again. Also the typical smell was there… I gave a robe. The result: renewed recurrence of Clostridioides Difficile.
Clostridioides – 2nd relapse
After the second relapse, I was about to go crazy. I was scared to death and worried if I would ever live a normal life again. On the other hand, you also get a certain routine and I decided not to go to hospital. I went to the family doctor. In the meantime, she had also informed herself more about the illness.
We decided to go back to VANCOMYCIN and approach the matter. This time not only 10 days, but also a slow end of the medication.
I was also referred to an internist to do a colonoscopy on me. This appointment took place shortly before the end of the 10 days on which I took the full dose of VANCOMYCIN. The internist said after the examination that my intestine looked “clean”. He found no signs of excessive colonization with Clostridioides Difficile bacteria. So no white coating on the intestinal wall. He said that it might not be the bacteria that caused the diarrhea. Instead, I could have developed a irritable bowel syndrome through the many antibiotics recently. In his opinion, I could stop Vancomycin.
In such situations I was totally desperate. Every doctor tells you something different. What to do? Weaning? But who tells me that I won’t experience the same thing again as with the last relapse? Why should the 10 days of VANCOMYCIN work this time?
That was a very stressful time for me. Above all, I wasn’t sure whether the doctors really knew exactly what they were doing. In addition, Clostridioides is always associated with relatively high relapsing probabilities. Therefore, it is never really possible to make certain statements about when they will be defeated.
Fortunately, my family doctor was always honest. She openly admitted that she didn’t know so much about Clostridioides. In the meantime, she had taken the trouble to discuss the disease with her colleagues as well as with the staff of the chair analysis laboratory. She also researched information on the treatment of the disease. Together we then designed a therapy that ultimately proved effective.
Clostridioides – Successful therapy
In the course of this text I have always given information about the properties of Clostridioides Difficile. Here are some additions and a short overview, so that you can understand why I took which measure:
Clostridioides encapsulate themselves. This means that they can decapsulate again after antibiotic therapy and then multiply again. => So we decided to take VANCOMYCIN for a longer period of time.
In the intestinal flora there is a competition among the microorganisms. Unfortunately, the good bacteria in my intestinal flora were strongly decimated. => Therefore I decided to feed myself a number of bacterial cultures that belong in a healthy intestinal flora. I wanted to increase their population so that the Clostridioides could no longer spread unhindered.
Natural enemies of Clostridioides are lactic acid bacteria. They prevent their growth by creating an acid environment where they cannot survive. => Yoghurt, buttermilk and kefir were therefore now on the menu more frequently than before.
The various strains of Clostridioides bacteria feed on either carbohydrates (sugar) or protein – preferably meat. They are also responsible for meat rot and produce life-threatening nerve toxins. Some of them are so dangerous that they used to serve as arrow poisons for the Indians. => I changed my diet so that I took almost no sugar. In addition, for many weeks I almost completely renounced meat. So I simply wanted to deprive them of their food so that they would no longer thrive so well.
Every bacterium and every fungus prefers one or the other source of food. Therefore I wanted to supply the good microorganisms with the optimal food. Many useful intestinal bacteria grow particularly well when they are surrounded by fibre.
Water – The be-all and end-all for building intestinal flora and for intestinal recovery. It is highly advisable to drink very much during the existence of the disease. It is best to only drink still water from the tap or bottle. 3 litres a day are a good guideline in any case.
Conclusion:
The problem with such bundled measures is that if they are successful, it is never possible to say exactly which means are responsible for the success. But perhaps it is also the case that it would not have worked without precisely this combination. Therefore, I can only speculate subjectively that in some relapses it may actually fail because the effect of METRONIDAZON or VANCOMYCIN is sufficient to decimate the Clostridioides. But the rest of the intestinal flora recovers so slowly after ingestion that in the end it is they again who win the race for the habitat. I don’t know for sure, but it fits in with what you learn in biology at school and what information I found based on my research.
So here you can see my subjective treatment plan that worked for me. This is without guarantee and without guarantee.
Long-term antibiotic therapy
I took the VANCOMYCIN 10 days in full dose. After that the dose became smaller and smaller. Towards the end I only took tablets every 2-3 days. So we made sure that the encapsulated germs were decapsulated and then killed. Their share of the intestinal flora should be reduced more and more.
The long-term therapy lasted a total of 66 days.
10 days – 4 x daily 125 mg VANCOMYCIN
7 days – 2 x daily 125 mg VANCOMYCIN
14 days – 1 x daily 125 mg VANCOMYCIN thereafter
7 times – every 2 days – 1 x daily 125 mg VANCOMYCIN thereafter
7 times – every 3 days – 1 x daily 125 mg VANCOMYCIN
If you take a strong antibiotic for such a long time, eat hardly any sugar or meat, your body feels very emaciated. I lost 15 kg of body weight. It was a terribly hard phase in my life, which was accompanied both physically and psychologically with very high loads.
Rebuilding of the intestinal flora
The following preparations help to rebuild a healthy intestinal flora:
- Mutaflor
- Symbioflor 1
- Perenterol (not taken at the time)
- inulin
- Combi Flora SymBIO
- Yoghurt / Buttermilk / Kefir
All these remedies can be bought on the German Amazon website. Or maybe in EU-wide pharmacies.
Mutaflor
These capsules contain high doses of bacterial cultures of the strain E.coli Nissle 1917. In the First World War it was discovered that soldiers were more resistant to intestinal diseases, in which this strain colonized the intestines in high proportions.

Mutaflor is also a very popular remedy among people with ulcerative colitis.
Symbioflor 1
Symbioflor is a preparation containing cultures of Enterococcus Faecalis bacteria.
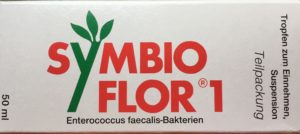
They also belong to the “good bacteria” that we need in the intestinal flora.
Perenterol
Perernterol contains a number of dry yeast cultures that should be found in the intestinal flora.

I did not take it during my illness, but some doctors recommend it as an accompanying medication when taking antibiotics. It seems to help prevent the spread of Clostridioides from the very beginning. Had I known this earlier… 🙁 – If it was true, it would have saved me a lot of grief and pain.
Inulin
Inulin is a prebiotic fibre obtained from certain plant varieties. This preparation was recommended to me by my family doctor. She and another colleague in the practice regularly use it as part of their diet.
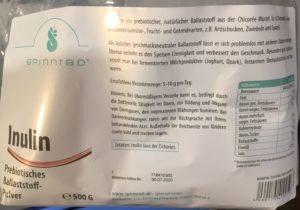
Correctly dosed, the product serves to provide good bacterial species with an ideal food environment for their growth. This increases their intestinal population somewhat faster.
Combi Flora SymBIO
Combi Flora SymBIO capsules contain a varied mixture of 13 probiotic bacteria and one yeast strain.

Their supply should also ensure that the number of “good bacteria” in the intestinal flora increases.
Yoghurt / Buttermilk / Kefir
Yoghurt, but especially buttermilk and kefir contain lactic acid bacteria (lactobacilli) which survive permanently in the human digestive tract. These bacteria settle more easily in the intestine due to the increased intake. There they create an acid environment and serve as a kind of natural growth inhibitor for Clostridioides Difficile bacteria.
The end of the therapy
I took these drugs (except Perenterol) daily during my antibiotic therapy. Even after weaning, I continued to take them a few months later. I was simply very afraid that the Clostridioides would return. It took months for me to have sufficient confidence in my intestinal flora. But over time it turned out that I had won the fight this time.
Alternative antibiotics
As additional information I would like to mention that there is a seemingly very effective antibiotic which can also be used against an infection with Clostridioides Difficile: FIDAXOMICIN (trade name: DIFICLIR)
FIDAXOMICIN is even more expensive than VANCOMYCIN. 20 pieces of DIFICLIR with 200 mg cost about 1.800-2.000 Euro. They are therefore about 9 to 10 times as expensive as VANCOMYCIN.
The “Joint Federal Committee” of Germany has attested him an additional benefit compared to VANCOMYCIN against the pathogenic C.Difficile. The better effect, however, only appeared in severely ill patients.
I suspect it is very unlikely that the health insurance company will allow a doctor to prescribe this drug unless there is a very important reason. In my desperation I had even thought for a short time to pay out of my own pocket if the VANCOMYCIN had not worked in the second therapy.
Clostridioides – Last resort stool transplant?
If all this hadn’t worked, probably only one solution would have been possible. There is a procedure called stool transplantation. As a patient, the complete intestinal flora of a healthy person is transferred. I didn’t try it myself, but I had already called a clinic in Starnberg (Germany) and informed myself about it. It works something like this:
From the bowel movement of an intestine-healthy donor, the bacteria are settled and bred in a culture. This means that you simply multiply what is already contained in the “cocktail”. Of course, everything is cleaned so that you only find a clear liquid at the end.
This liquid contains a lot of intestinal bacteria in a healthy mixture. It is pumped into the intestine with the help of endocopic procedures. The good bacteria immediately accumulate on the intestinal wall and virtually displace the Clostridioides. The infection comes to a standstill immediately and the patient is cured. The success rate for stool transplantation is about 90%.
By the way, the idea is not as new as you might think. In ancient China as well as in North Africa it was already common centuries ago to give patients with diarrhoea oral dung to fellow humans or animals.
In addition to the clinic in Starnberg, there is also the University Hospital in Cologne (Germany), which is also active in this field. Here one should investigate however if necessary again and again times. It is quite possible that there are other clinics that offer this procedure.
But as I said, I emphasize that I have no experience with this myself. I had only considered it as the last option if the interval therapy had failed.